TLEMsafe
TLEMsafe – Improving safety and predictability of complex musculoskeletal surgery using a patient-specific navigation system
The aging of population results in high and still growing numbers of cases of musculoskeletal diseases as well as prosthetic revision operations. Highly invasive and complex surgical interventions are unsafe, uncertain in outcome and have a high complication rate. Information and Communication Technologies (ICT) are often used to aid surgeons plan and/or conduct the operation. Often they use medical imaging data of a certain kind – usually computed tomography (CT) or magnetic resonance imaging (MRI). Rarely, however, they take advantage of information acquired with use of multiple (more than two) measurement modalities.
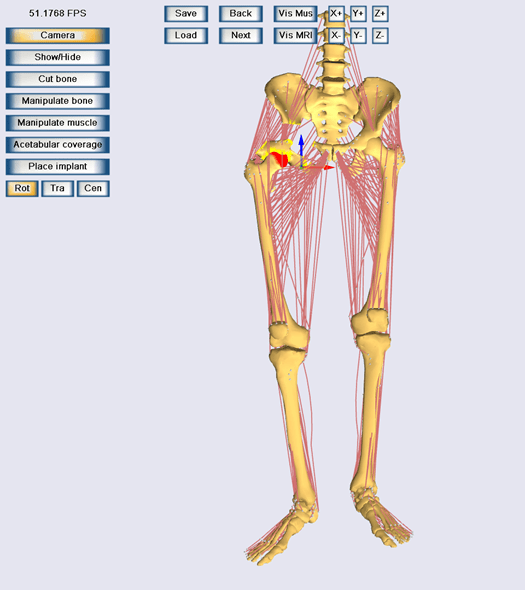
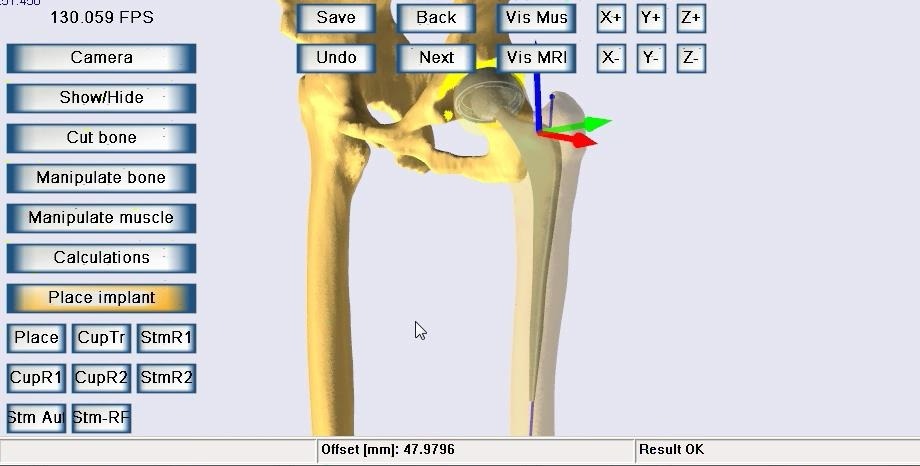
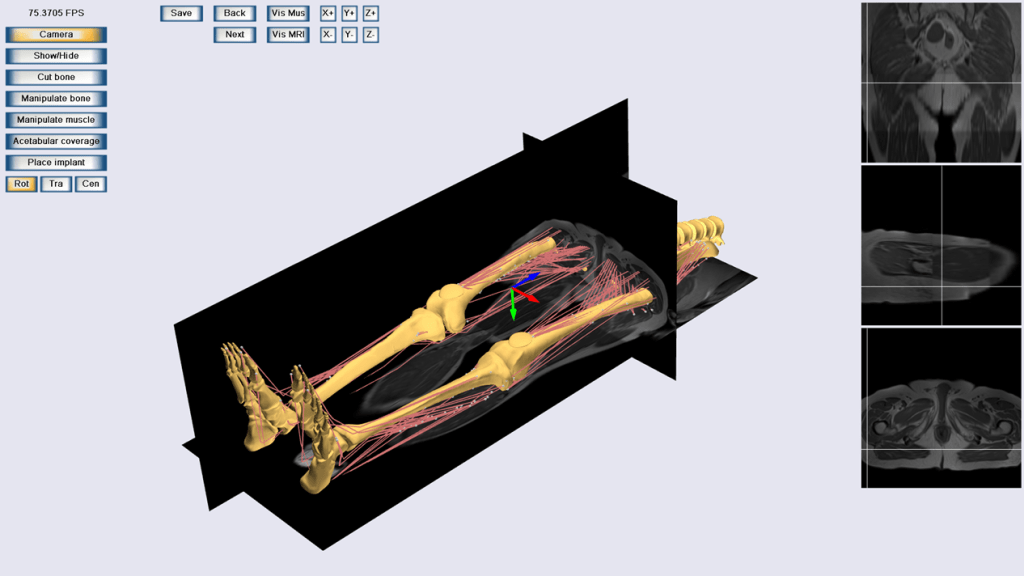
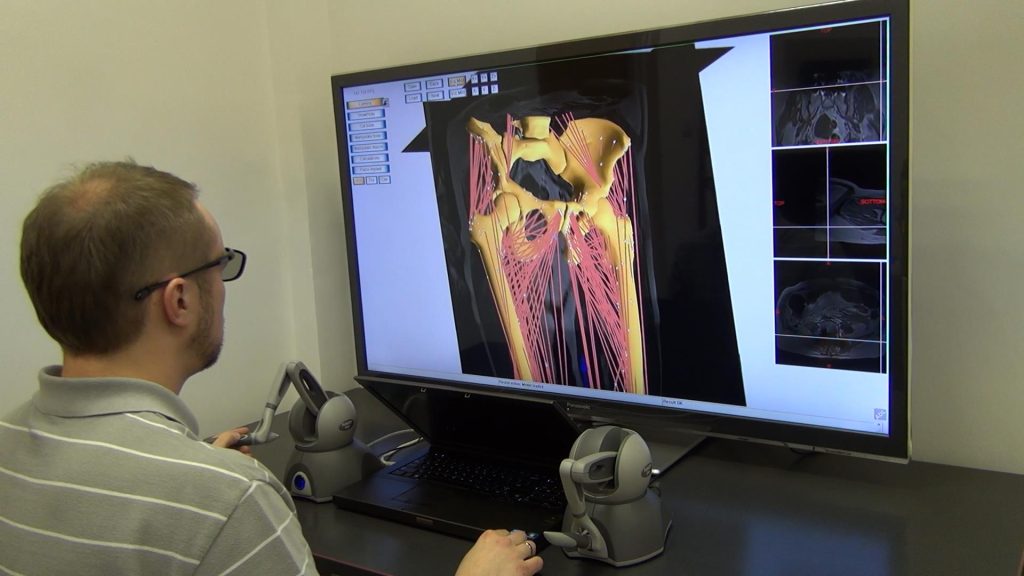
The aim of the TLEMsafe project was to create a patient-specific surgical navigation system, based on innovative ICT tools, for training, pre-operative planning and execution of complex musculoskeletal surgeries of lower limbs. A number of methods were developed within the project, oriented at helping the surgeon to safely reach the functional result optimal for the patient. The system may also serve as a user-friendly training for surgeons.
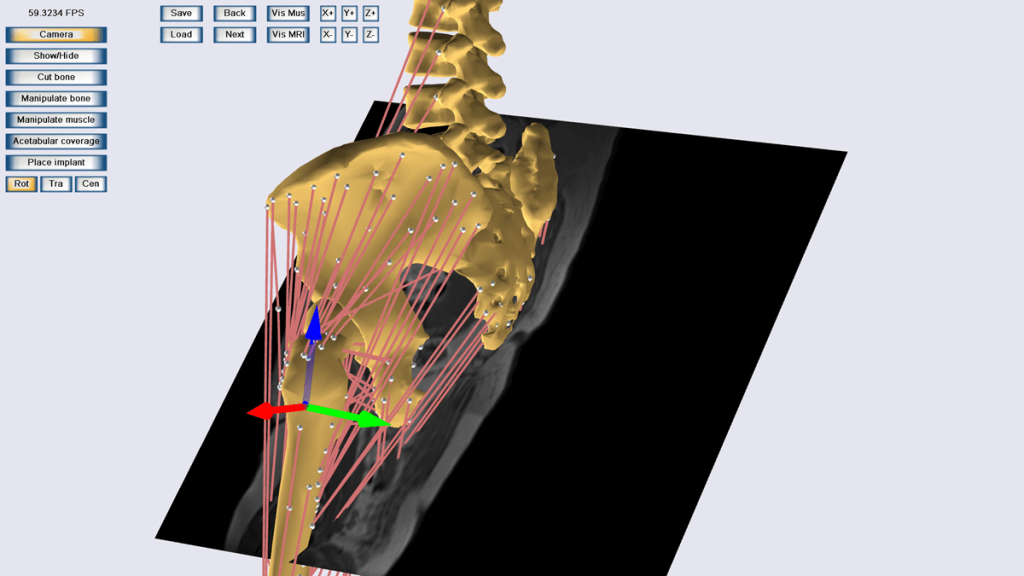
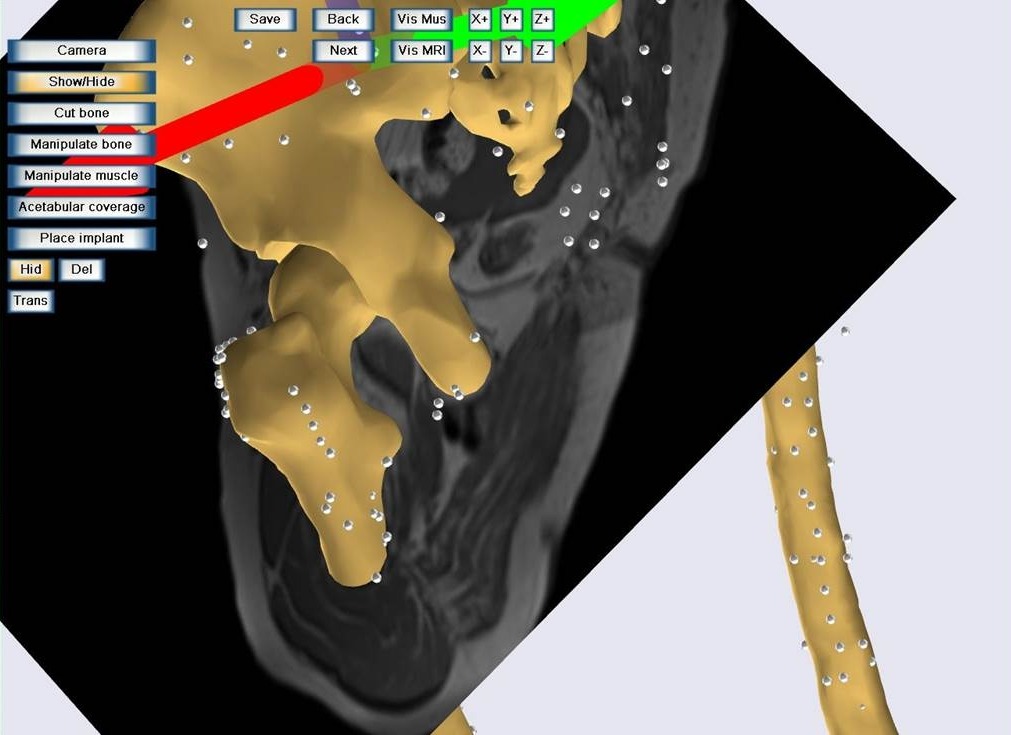
A detailed and reliable dataset describing the specific patient’s musculoskeletal system is acquired so as to provide the most comprehensive ground truth for further processing. Three-dimensional (3D, static) and four-dimensional (3D + time, dynamic) medical imaging techniques are used to adjust standard parameters describing the lower limbs so as to imitate the subject’s biomechanical condition.
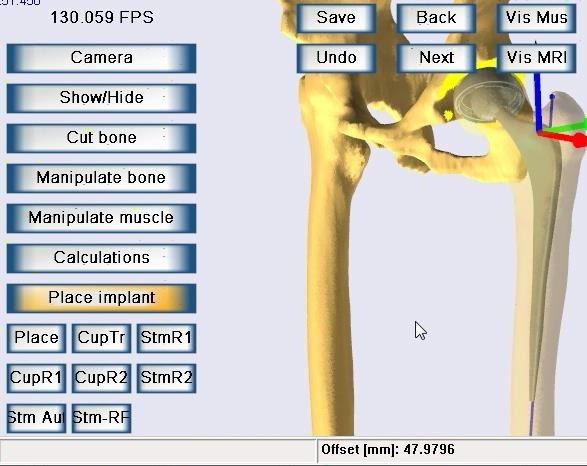
The surgery planning procedure is performed with use of SPE3D (Surgery Planning Environment 3D, pronounced speed) application that was developed at Virtual Reality Techniques Division, WUT. It is used to modify the patient-specific model according to one or more surgical scenarios driven by the operator (a surgeon or a student being trained). Essential in SPE3D is the fact that the operator is provided with a multimodal 3D model that may be modified in a clinically relevant manner. The changes committed by the operator lead to a change of the model parameters. Modified parametric models are analyzed with a biomechanical tool which allows estimation of the functional effects of the changes of the model parameters. In this way the functional outcome of the patient can be estimated for every individual surgical scenario. The optimal plan may be fed into a surgical navigation system that allows the surgeon to reproduce the selected plan during the actual surgery.